Diabetic retinopathy
Diabetic Retinopathy refers to a condition in which the retina gets affected by diabetes, which leads to destabilized blood vessels. Many diabetic patients suffer from this disease in which a change in retinal blood vessels results in loss of vision. Weakened blood vessels may leak fluid or blood, causing damage to the retina.
Symptoms
In most cases Diabetic retinopathy MAY NOT produce any significant symptoms in the early stages. Therefore, bi-annual (6- monthly) eye check-ups are highly advisable for diabetic patients. However, the some symptoms include:
- Gradually worsening vision
- Sudden vision loss
- Shapes floating in your field of vision (floaters)
- Blurred or patchy vision
Causes
- Diabetes mellitus especially over a prolonged period
- Poorly controlled diabetes mellitus
- Damage caused by diabetes to the tiny blood vessels in the retina (retinal-microangiopathy)
Diagnosis
- Fundus Fluorescein Angiography (FFA): After pupil dilation, Fluorescein dye is injected into the vein in the arm. Photographs are then taken from a specialized camera. Dye will not leak out of normal blood vessels, if it is leaking, it means the vessels are damaged.
- Optical Coherence Tomography (OCT): This is the test to measure the amount of swelling on the retina, particularly on the area where the image is formed. It is also useful to monitor the progress of patients.
Treatment
- Intravitreal injections: Injections are used to reduce the retinal swelling, prevent formation of new blood vessels and stabilise/improve the vision of the patient. These injections may be required in multiple doses and repeated whenever the swelling increases. Intravitreal injections are also administered prior to retinal surgery to avoid excess bleeding.
- Retinal laser photocoagulation: Photo coagulation of damaged areas due to diabetic retinopathy is done with green laser. This treatment is done to stabilise vision and is effective in most patients. It helps to seal the leaking blood vessels and prevents growth of harmful new blood vessels. Aim is to regress bad new vessels and reduce the long-term chance of bleeding, retinal detachment and visual loss. Retina laser treatment may be performed over multiple sittings depending on the severity of the disease.
- Vitrectomy (Vitreoretinal Surgery): These surgeries are required in advanced cases of diabetic retinopathy with severe damage to the retina, retinal detachment or bleeding inside the eye cavity. Vitrectomy or vitreoretinal surgery aims to remove the abnormal amount of blood collected in the eyes and to remove the scar tissues over the retina as well as settle the retina in cases of diabetic retinal detachment.
ARMD
Macular Degeneration is a condition in which the central retina, called macula, starts to deteriorate and causes blurring of central vision. It is often called age-related macular degeneration (ARMD) as the vision impairment progresses as the patient ages. It is usually seen in older people.
Types
Dry Macular Degeneration: new blood vessels do not form
It is the more common type of the disease. It is also the less serious type of the two. There is a slow atrophy/degeneration of the macula. Because the degeneration process is slow, vision loss is gradual.
Wet Macular Degeneration; new blood vessels are formed
This is more serious. It forms when blood vessels grow under the macula. They leak fluid or blood and blur the central visio. Vision loss can occur immediately or within days.
Symptoms
- Difficulty in recognizing faces
- Visual distortions such as straight lines appearing bent
- Blurring of central vision despite use of glasses.
- Difficulty in judging heights or distances
- Need for brighter light when reading or doing close work
- Colors appear less bright.
Diagnosis
- Vision test (visual acuity)
- Dilated Retina Examination
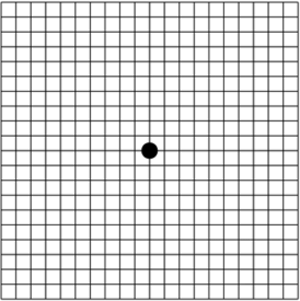
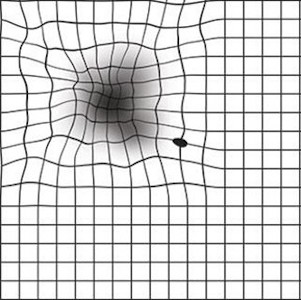
- Amsler Grid: The pattern of the grid resembles a checkerboard. You will cover one eye and stare at a black dot in the center of the grid. While staring at the dot, you may notice that the straight lines in the pattern appear wavy. You may notice that some of the lines are missing. These may be signs of AMD.
Amsler grid seen by normal people
Amsler grid seen by patients of ARMD
- Fundus Fluorescein Angiogram helps to differentiate between dry and wet forms of ARMD. In this test special photographs of the retina are taken after injecting fluorescein dye.
- Optical Coherence Tomography helps us to locate the Choroidal neovascular and Sub retinal Neovascular Membrane in wet ARMD and find out if there is any swelling in the macula.
Treatment
Dry Age-Related Macular Degeneration
Nutritional supplements: There is no definite treatment for the dry ARMD but a specific high dose formation of antioxidants, Beta Carotene and zinc reduces the risk of advanced AMD. They may help to maintain their vision. A healthy diet rich in green leafy vegetables and fish. Avoid smoking. Maintain normal BP Exercise and avoid obesity. If you have lost sight from AMD do not be afraid to use your eyes for reading, watching TV.
Wet Age-Related Macular Degeneration
- AntiVEGFs injections: These are substances that stop leaky blood vessels from forming or growing. They are given to patients suffering from wet ARMD. There are 3 drugs currently available, Avastin, Accentrix, Eylea. These are injected in the affected eye, often a course of atleast 3 injections at monthly intervals. Accentrix and Eylea are safer in cardiac patients.
- Photodynamic Therapy (PDT): Certain types of Wet ARMD were earlier treated with Photodynamic Laser therapy using an injectable dye called Verteporfin. Nowadays, it is reserved for Non responding Wet ARMD cases.
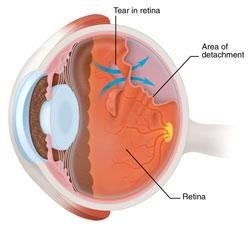
Retinal Detachment
A retinal detachment refers to a situation in which the retina is separated from its attachments from underlying tissues within the eye. Mainly retinal detachments are an outcome of a retinal tear or break. Retinal detachment is a sight-threatening eye problem that may occur at any age although it usually occurs in middle-aged or older individuals. Retinal detachment is a very serious problem that almost always causes blindness unless treated.
Symptoms
- Decrease/blurring of vision
- Appearance of a curtain-like shade/shadow in the field of vision
- Shapes floating in your field of vision (floaters)
- Flashes (Flashing lights or flashes of lightning in peripheral field of vision)
Retinal detachment is not painful. Sometimes symptoms of flashes and floaters are not due to a tear or detachment, and can simply be because of separation of vitreous gel from retina. This condition is known as posterior vitreous detachment (PVD).
Causes
The eye is filled with vitreous, a jelly-like substance. This is attached to the retina in several places around the back wall of the eye. As we get older the vitreous shrinks and its consistency becomes more watery. As it shrinks, it may pull a part of the retina, resulting in a tear or hole in the retina. Retinal tears increase the chances of retinal detachment, most detachments are caused due to one or more tears or holes in the retina.
Treatment
Surgery is a highly successful treatment, and if done in time, can restore good vision.
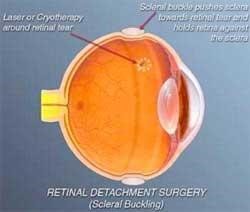
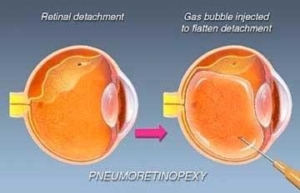
| Scleral Buckling | Laser photocoagulation and/or Cryopexy (freezing) | Pneumatic retinopexy | Pars Plana Vitrectomy |
|---|---|---|---|
| In this retinal detachment surgery, surgeons suture a silicon material to the sclera. This buckling indents the eyewall to a position where it allows the retina to re-attach. This procedure is usually combined with placement of an encircling silicone band around the circumference of the eye to lessen the pulling of the vitreous on the retina. These buckles and bands are left permanently and are not visible from outside. Usually combined with cryopexy for sealing the retinal tear and settling the detached retina. | Both done in the initial stages of Retinal detachment when only a retinal break is present with a minimal area of detachment. The retina specialist will put a laser beam into the eye to create a burn around the retinal tear. The burn creates a scar sealing the retina to the underlying tissue. The retina specialist may also perform cryopexy which involves applying extreme cold/ freezing temperatures to achieve the same results. | Pneumatic retinopathy involves putting a gas bubble in the eye in a way that pushes the retina to its original position. This retinal detachment treatment is usually done with laser surgery/cryopexy to ensure the retina stays in its right position permanently. The patient is instructed to keep his or her head in a specific position so that the gas bubble seals the retinal tear. Circulation of fluid through the tear stops and the retina is re-attached | In this surgery, micro incisions are made in the eye through which micro-instruments are inserted by retina surgeons to complete the procedure and reattach the retina. At the end of the procedure, silicon oil liquid or a specialised gas is left within the eye cavity to provide support to enable attachment of the retina. With the advancement in medical technology, this surgery is one of the most common for complex retinal detachment. If silicone oil has been used, it has to be removed at a later date as a separate surgical procedure. The surgery may take several hours. |
Retinopathy of prematurity (ROP)
Retinopathy of prematurity (ROP) refers to a potential blinding eye disorder that mainly affects premature infants. The lower the birth weight the more are the chances that the baby will suffer from ROP. This disorder generally develops in both eyes and is one of the most common causes of visual loss in childhood that leads to lifelong vision blindness and impairment.
Risk Factors
- Preterm Delivery
- Low Birth weight
- Oxygen supplementation at birth
Causes
ROP occurs due to the growth of abnormal blood vessels in the retina. Retinal detachment may occur when these abnormal blood vessels scar the retina due to which it gets pulled out of its position. Retinal detachment is one of the main causes of visual impairment and blindness in ROP.
Screening
Babies should be screened before discharge from the NICU or 30 days of age, whichever is sooner.
Treatment
- Laser therapy: The most effective way to treat ROP is laser therapy. In Laser therapy, the peripheral retina, which has no normal blood vessels, is burnt away.
- Retinal Detachment Surgery: Vitrectomy is the most preferred surgical operation that is used for preventing retinal diseases. In this operation, the retina is attached back in its normal position. This procedure lasts for long hours due to which you can get hospitalized for certain hours.
Vascular Occlusion
This occurs due to a blockage of the blood vessels which serve the retina. This in turn leads to bleeding and leakage of fluid occurs from the area of blocked blood vessels.
There are two types of vascular occlusions:
- Arterial occlusions
- Venous Occlusions (more common)
Symptoms
- Usually there is sudden painless loss of vision.
- Diagnosis can be made after an dilated eye examination
Causes
- High Blood Pressure (hypertension)
- Heart Problems
- high cholesterol
- Diabetes
Diagnosis
- OCT: It is a useful non-invasive test for diagnosing edema or swelling on the centre of the retina due to vascular occlusions.
- Fluorescein Angioigraphy: It is also performed to get to know about blood supply and to determine any growth of new abnormal blood vessels in these eyes.
Treatment
- Intravitreal AntiVEGF injections are given to treat macular edema (swelling in the retina)
- Steroid injections/implants are given in case of a resistant macular swelling
- Laser therapy: Photocoagulation therapy is done in areas where the blood supply to the retina is affected.
These treatment modalities may have to be repeated frequently depending on the patient’s response to therapy.
FAQs
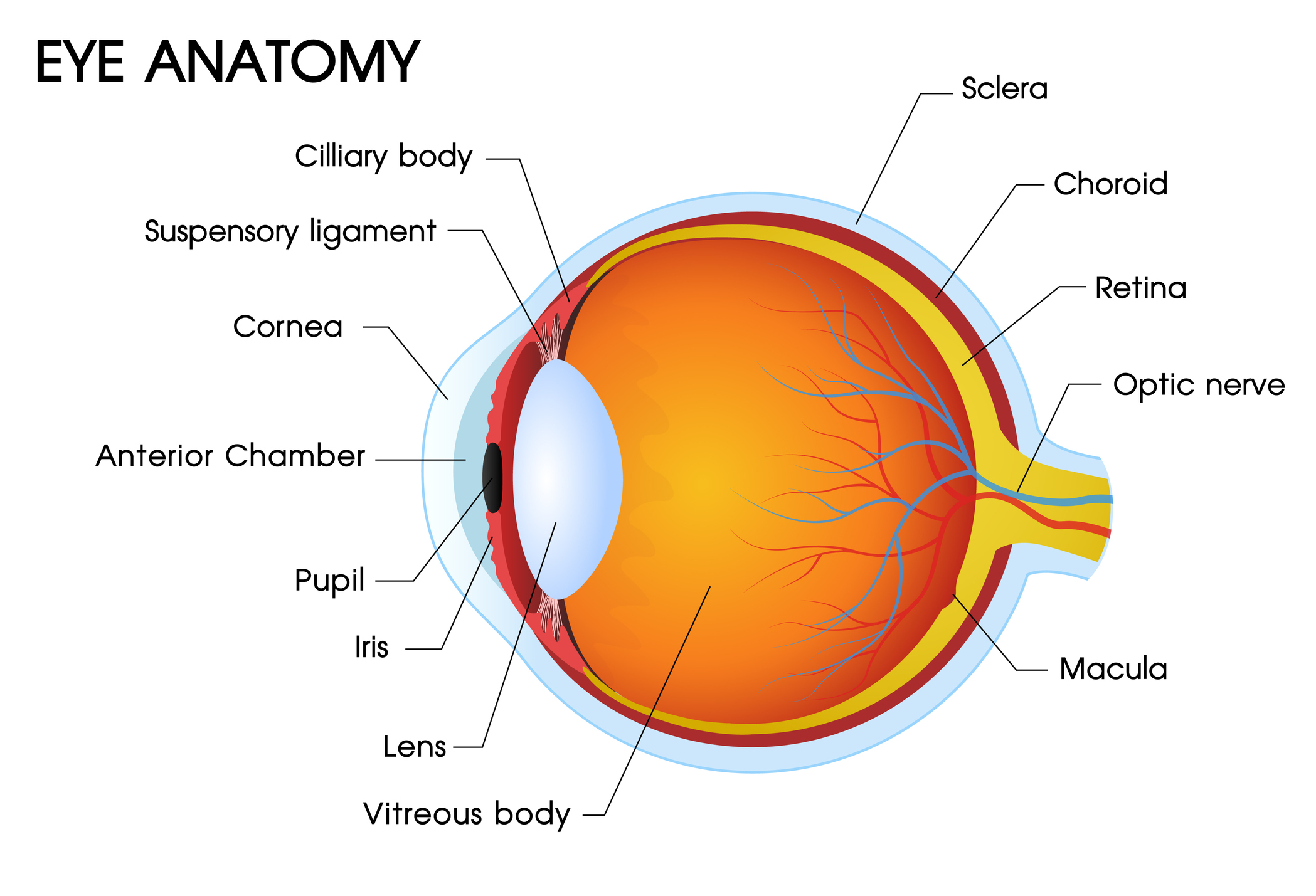
What is Retina?
The retina is an extremely thin-layered tissue that is positioned at the inner back surface of the eye. The image is formed onto the retina by focusing of light by both lens and cornea. This light which strikes the retina causes a flow of electrical and chemical signals that eventually activate nerve impulses and as a result of this, generates an electrical retort in other layers of retina. These electrical signals are then sent to various visual centers of the brain through fibers of optic nerves. When these electric signals enter specific areas of our brain, it allows us to see and also to understand what we are seeing. The size of the retina is about a postage stamp.
Retina comprises a layered structure that has several layers of neurons which are interconnected by synapses. Macula is the central part of the retina. There are two types of light receptor cells located within the retina which are known as cones and rods. Rods permit us to see in situations of compact illumination. Cones supply us with color and sharpness of vision.
What are the risk factors involved with retinal disorders?
Risks factors involved with retinal disorders can be:
● Ageing
● Smoking
● Diabetes and Hypertension
● Eye trauma
● Obesity
● A family history of retinal diseases
What are Floaters?
Floaters are frequently described by patients as strands, spots, or little flies/worms, and are caused because of condensations in vitreous gel.
How does diabetic retinopathy progress?
Diabetic retinopathy progresses in the following 4 stages:
- Mild Non-proliferative Diabetic Retinopathy (NPDR)
- Moderate Non-proliferative Diabetic Retinopathy
- Severe Non-proliferative Diabetic Retinopathy
- Proliferative Diabetic Retinopathy (PDR)
What kind of eye problems does vitrectomy surgery treat?
Vitrectomy surgery is done to treat eye disorders like:
● Diabetic vitreous haemorrhage
● Retinal detachment
● Macular hole
● Proliferative vitreoretinopathy
● Endophthalmitis
● Removal of Intraocular foreign body
● Epiretinal membrane
● Retrieval of the lens nucleus following complicated cataract surgery
What are the complications of vitreoretinal surgery?
Even though the vitreoretinal surgery for retinal detachment is generally successful, there can be some complications.
There can be temporary problems like drooping of the upper lid and double vision. More serious but very infrequent complications include bleeding that is severe enough to interfere with vision, infection, glaucoma and cataract formation. In such cases the surgeon will discuss with you the possibility of a re-operation to successfully re-attach the retina. However it is important for the patient to know that there is a chance that the surgery may fail due to the abovementioned serious complications, or due to the progressive nature of the retinal disease.
What happens after vitreoretinal surgery?
Vitreoretinal surgery is usually done on an outpatient basis. The eye specialist may prescribe antibiotic and anti-inflammatory eye drops for a few weeks after the surgery. This surgery has a high success rate.