Symptoms
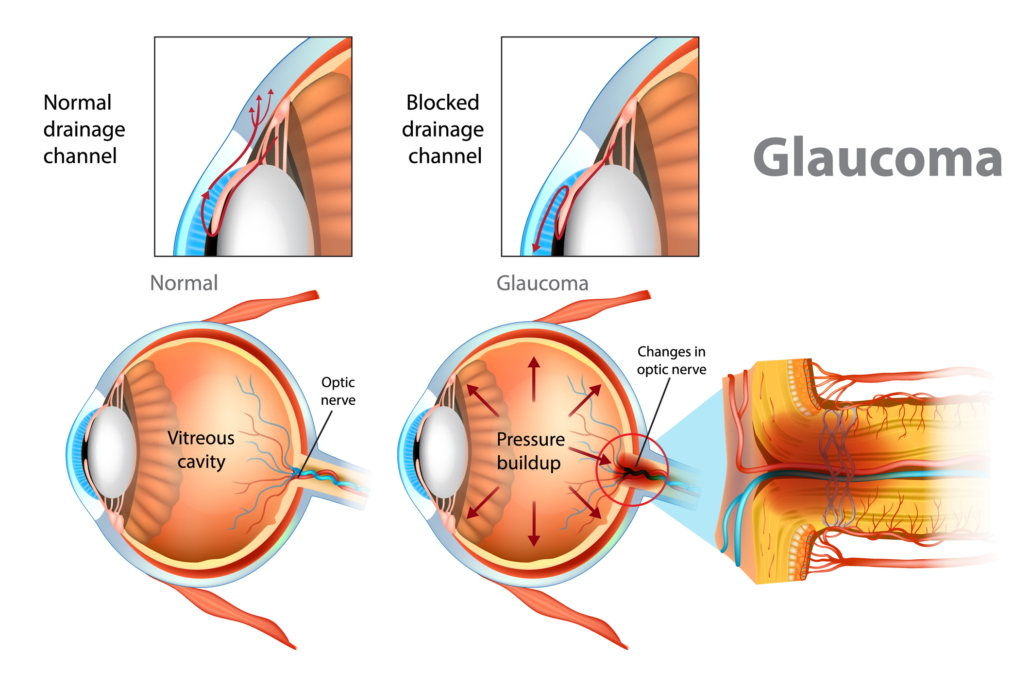
Glaucoma is also known as a ‘silent thief of vision’ as there may be no significant symptoms in early stages of Glaucoma, and therefore it may go undetected. Some symptoms to look out for are:
- Mild eye-ache or evening headache, especially in the evening and in dim light conditions
- Redness and pain in the eyes
- Slow often unnoticed decrease of vision
- Rapidly changing glass prescription
- Reduced vision in low light conditions or at night
- Seeing colorful haloes or rings around bulbs
- Difficulty in viewing objects in peripheral vision
Who is at risk
- Age: Patients above the age of 40 years
- Family history of Glaucoma
- Medical history: Patients with hypertension, migraine, diabetes, long term use of steroidal medications, previous eye injuries
- Patients having high powered glasses (plus or minus)
Treatment
Evaluation
The examination includes an evaluation of the patient’s vision, eye pressure (IOP), and the optic nerve with dilation if appropriate. Additionally, a visual field test, optic nerve imaging and gonioscopy (testing of the fluid drainage angle) may also be conducted.
Glaucoma Diagnosis
- Tonometry / IOP measurement / Eye pressure measurement – An average pressure ranges about 10 to 20 mm of Mercury. Some patients may have high IOP but do not have glaucoma
- Gonioscopy – Testing of the fluid drainage angle to rule out Angle-Closure Glaucoma
- Dilated Ophthalmoscopy – The pupil is dilated to inspect the optic nerve at the back of the eye
- OCT (Optical Coherence Tomography) – To evaluate the structural parameters of the Optic Nerve Head (ONH). The parameters are Retinal Nerve Fibre Layer (RNFL), Ganglion Cell Complex (GCC) and Cup Disc Ratio (CDR)
- Perimetry / Visual Fields Test– To evaluate the peripheral field of vision
- Optic Nerve Imaging – To document the status of the optic nerve
- Pachymetry – The corneal thickness is measured for accurate IOP measurement
Treatment
Medication – Glaucoma is most commonly managed by medications in the form of eye-drops, tablets and syrups. These are prescribed to reduce the eye pressure/ IOP.
Laser – Laser treatment is based on the patient’s type and stage of glaucoma
Surgery – Surgery is recommended for patients with glaucoma which is unresponsive or uncontrolled with medicines and lasers
Laser
YAG Laser Peripheral Iridotomy (YAG PI): Performed for patients with Angle-closure Glaucoma. It is performed usually on both eyes to prevent an acute rise in pressure or an ‘attack’ of glaucoma. A small laser incision is made on the iris to create a new path to drain the eye fluid. It is a relatively quick OPD procedure done using anesthetic eye-drops.
Selective Laser Trabeculoplasty (SLT): Performed for patients with Open-Angle glaucoma. A special laser is used which does not cause any burns inside the eyes. The autoimmune system of eyes is stimulated so as to clear blockage in the drainage passage without causing damage to surrounding tissues. This is a painless process and gets completed in just a few minutes using anesthetic eye-drops.
Diode Laser Cycloablation: This procedure is performed for advanced glaucoma. A specialised laser is applied on the fluid production portion of the eye so as to reduce the fluid production and therefore control eye pressure.
Surgery
In cases where medications and laser treatments prove to be ineffective or are found to be inappropriate, surgical operation is performed.
Trabeculectomy: Trabeculectomy (or Trab) is the standard procedure for advanced and uncontrolled glaucoma. The surgeon creates an alternative opening in the drainage channel for the eye fluid to control the eye pressure. Most patients don’t require medication post-surgery. However for few patients who do require medications, IOP is managed more easily with the help of surgery.
Glaucoma Drainage Devices (GDD): Drainage implant surgery is sometimes performed when a person is not suited for Trabeculectomy or where Trabeculectomy has failed. A tiny tube is inserted into the eye through the sclera serving as a path for fluid to drain away. The other end of the tube is attached to a tiny reservoir on the surface of the eye (between the eye muscles, so it is not visible) to hold the fluid until it is absorbed into the surrounding tissue.
FAQs
Which age does glaucoma affect?
Glaucoma is most common after age 40, but it may affect any age group. Congenital Glaucoma affects newborn or children.
How often should one get an eye check up for glaucoma screening?
- After the age of 40 years, one should get an eye check up for glaucoma every 3 to 4 years even if there are no symptoms.
- If a family member has glaucoma, if you have diabetes, if you are on long term systemic steroids for some other disease, or if you have suffered a blunt eye injury in the past, you must get your eyes checked every 1 to 2 years.
My vision is good, so then why do you say I have glaucoma?
A Central vision is lost only in the very late stages of Glaucoma. It starts with damage to your peripheral vision and gradually comes to the centre. By the time the central vision gets affected, it’s too late to restore vision. In a way, good vision is misleading as far as severity of glaucoma and extent of damage is concerned.
How serious is my glaucoma problem?
This depends on the amount of optic nerve damage. This is measured by VFA (visual field analysis) and GDx (which measures the thickness of the nerve). As the damage is permanent, the right measures should then be taken to prevent or slow down further damage.
Is glaucoma preventable?
Glaucoma is not curable, however damage due to it is preventable with the right treatment. But the damage that has already happened due to Glaucoma cannot be reversed. Glaucoma is a life-long illness and needs regular follow ups and treatment.
Is Glaucoma hereditary?
Yes, Glaucoma can be hereditary. People who have a family history of Glaucoma should get their eyes tested to rule out Glaucoma.
Can I get back my side vision after treatment?
Unfortunately the vision loss caused by glaucoma is permanent and cannot be regained.
What precaution can one take to prevent Glaucoma?
People who are at the risk of developing glaucoma should undergo regular eye examinations. Diabetics should ensure good control of blood sugar levels. Avoid smoking. Avoid drinking 2-3 glasses of water at a time.
Do I need to come for follow ups after laser / surgery?
Treatment of glaucoma is life-long. Even after laser or surgery one may need additional medication and follow ups throughout life to monitor the progress of the disease.
Should and can one exercise with Glaucoma?
Exercise is good for the body. A patient of Glaucoma should exercise for at least 25 minutes, 3-4 times a week. You can do aerobic exercises like swimming, jogging, walking or ride a bike. Patients with advanced Glaucoma should avoid exercises like weight lifting or push-ups which cause a lot of strain. Certain yogic postures like shirshasana (where the head is below the body) are also best avoided.
What should glaucoma patients avoid?
Glaucoma patients should avoid taking steroids in any form and, if needed, must inform their doctor that they have Glaucoma. Do not self-medicate. Besides, avoid too much tea or coffee intake. Excessive coffee (more than 2-3 cups a day) is associated with elevated eye pressure and is best avoided. Avoid consuming large quantities of water/fluids in one go.
Can glaucoma occur in a baby?
Congenital Glaucoma may be present at birth or may develop shortly after birth. Such children may have large eyes which may appear bluish and tend to water, and have a tendency to avoid light (photophobia). It is more common in families where marriages occur between relatives and cousins (consanguinity). It needs immediate attention to prevent permanent damage to vision.
Does working on a computer or mobile worsen my glaucoma or eye pressure?
No, it does not. As long as you’re putting your eye drops regularly and getting check-ups done as required, you are free to use digital screens as much as you comfortably can. It is a good idea to take a break between long hours of work to prevent eye muscle fatigue.