Symptoms
- Gradually worsening vision
- Sudden vision loss
- Shapes floating in your field of vision (floaters)
- Blurred or patchy vision
- Eye pain or redness
Treatment
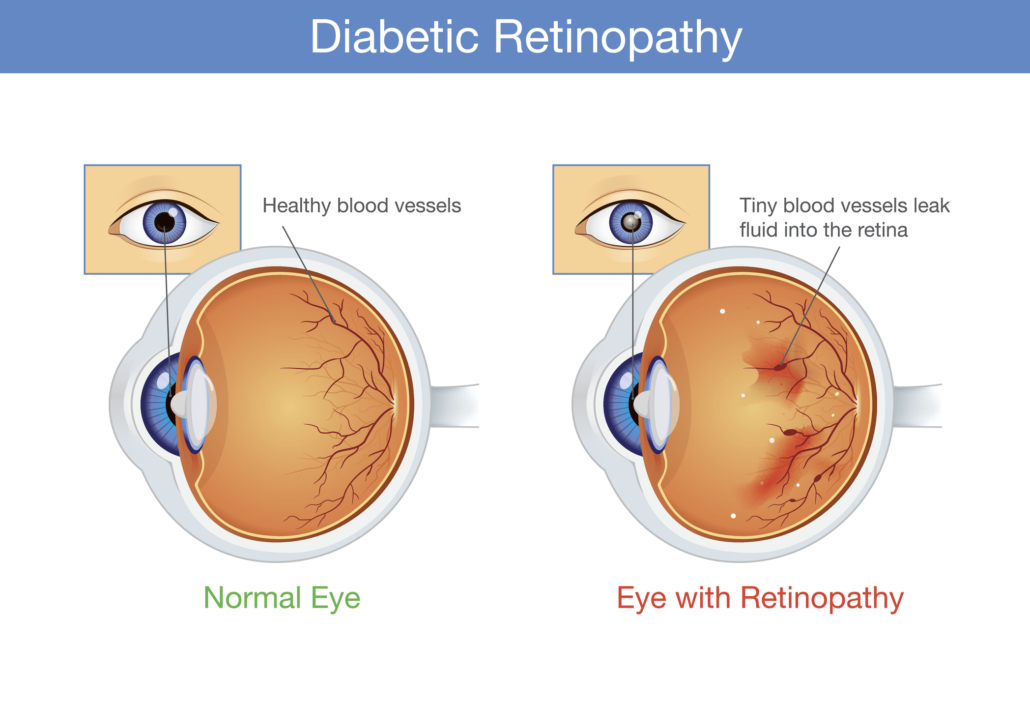
Detection of Diabetic Retinopathy
All patients with diabetes should get their eyes examined on a regular basis. Diabetic Retinopathy is detected through an eye examination that includes:
- Assessment of the visual acuity
- Retinal (Fundus) examination
- Intraocular pressure
- Fluorenscein angiography to detect abnormalities in retinal blood vessels
- OCT to detect swelling in retina
Diagnostic Tests
Fluorescein Angiography Test
This test is used to establish:
- Diagnosis
- Degree and extent of involvement
- Long term prognosis
- Need for Laser Treatment
- Baseline for follow up comparisons
Procedure
The pupils are dilated and then Fluorescein dye is injected into the arm. This dye circulates through the retinal blood vessel so that the small blood vessels can be easily seen. Photographs are then taken on the digital fundus camera. Dye will not leak out of normal capillaries, and if it is leaking it means the vessels are diseased.
OCT
This is a test to measure the amount of swelling on the retina, particularly the area where image is formed i.e. macula. It is also very useful to measure the progress of the patient.
Procedure
Pupils are dilated and scanning of retina is done through a beam through several sections and analysis is done.
Treatment
 There are various ways by which diabetic retinopathy can be treated which includes both surgical operations and laser treatments. Photocoagulation is one of the most used laser therapies for preventing growth of anomalous blood vessels. Lasers are created by a highly energetic and intense beam of light that helps in slowing down or even stopping progression of diabetic retinopathy in order to stabilize vision.
There are various ways by which diabetic retinopathy can be treated which includes both surgical operations and laser treatments. Photocoagulation is one of the most used laser therapies for preventing growth of anomalous blood vessels. Lasers are created by a highly energetic and intense beam of light that helps in slowing down or even stopping progression of diabetic retinopathy in order to stabilize vision.
Background retinopathy is mostly treated by using laser therapy. This therapy stops the leakage of fluid into the macula which results in stabilized vision. While in Proliferative Retinopathy two to three sessions of laser therapy is required. In this therapy atypical blood vessels are destroyed in order to minimize chances of severe vision loss. But one should notice that laser treatment is not a one- time procedure. Regular checkups and precautions are needed to be taken in order to prevent this disease.
Recently, along with laser treatment, certain medication when injected into the eye or just outside the eye has shown good results. These medicines include intravitreal Avastin, Lucentis as well as steroids. They often need to be repeated in order to keep the swelling in check. Being injected into the eye they are however to be used cautiously and judiciously.
Furthermore if the vitreous is too clouded with blood or there is traction retinal detachment, laser treatment will not work. In this situation, a surgical procedure called Vitrectomy needs to be performed. In this operation, the opaque vitreous gel is removed from within the eye by a special instrument that simultaneously sucks and cuts the vitreous.
FAQs
How is diabetic retinopathy diagnosed?
Tools like ultrasound, slit lamp, etc are used to assess whether a person is suffering from this disease or with any other eye problem.
How can we reduce the risk of diabetic retinopathy?
Loss of vision from Diabetic Retinopathy is largely preventable. Strict control of diabetes can reduce the risk of retinopathy by 40-60% and will also reduce the risk of other complications. You can reduce your risk or help prevent it getting worse, by controlling your blood sugar, blood pressure, cholesterol levels and kidney disease.
A large emphasis is placed on screening – that is looking for early signs of diabetes, often before the vision has altered and treating it at an early stage. Have a complete eye examination once a year or more frequently if advised, and get medical advice quickly if you notice any changes to your vision. Maintain a healthy weight, eat a healthy, balanced diet and exercise regularly and stop smoking.
Who is at risk for this disease?
- Patients with fluctuating, high and poorly controlled blood sugar levels.
- 10% of juvenile diabetics within 10 years, 50% after 15 years and 80-90% after 25 years.
- 30% of maturity onset diabetics within 5 years, 50% after 10 years and 70-80% after 25 years.
- Pregnant diabetic women
- Associated hypertension
- Family history of diabetic eye disease
Are there any side effects of Fluorescein Angiography?
Few patients develop nausea and occasional sickness that soon passes. Allergic reactions rarely occur. The dye has the effect of yellowing the skin for 3-6 hours and urine for 24 hours. Although the fluorescein doesn’t upset your diabetic control, you should continue to monitor your diabetes during this period.
Will the laser treatment hurt?
Normally laser treatment doesn’t hurt, but sometimes a dull thud sensation or occasionally a sharp pain is felt. A mild pain killer may be taken if required. If pain persists, report to your eye surgeon.
Will the laser treatment affect my vision?
Sight, following laser treatment, normally remains unaffected. Temporarily after treatment you will feel as if dazzled by light. Vision can be blurred for sometime. On rare occasions vision may worsen.